Technology & Innovation
The Pathway to Connectivity: The Operational Benefits of a Connected System
November 19, 2025 - Bayer in Radiology
Sponsored Content by Bayer in Radiology
In a rapidly evolving healthcare landscape, radiology departments face both significant opportunities and complex challenges with the integration of advanced technology. A recent expert panel at the AHRA 2025 Annual Meeting, featuring leaders from Bayer Radiology and UT Southwestern (UTSW), explored the transformative roles of connected contrast media injectors, workflow software, and operational artificial intelligence (AI) in the radiology suite.
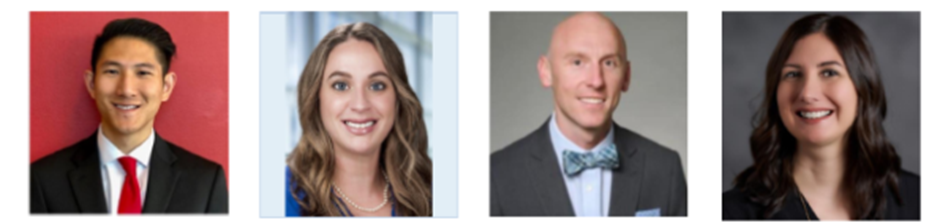
Panelists included Jason Le, Bayer Radiology global medical affairs lead, software as a medical device (SaMD) and injector software; Jessica Starkey, CT technical supervisor at UTSW; Jason Johnson, Bayer Radiology senior manager of informatics training; and Shawna Jones, Bayer Radiology associate marketing director. (Pictured below, left to right.)
Key Discussion Insights
Connected Injectors: Beyond Standalone Products
Connected injectors represent a major leap from traditional standalone injectors. As explained by Shawna Jones, these modern devices integrate seamlessly with hospital networks and imaging systems, serving not just as injection tools but as strategic assets in data-driven healthcare.
- Automated Data Capture: Connected injectors automatically log injection, patient, and protocol data, reducing manual error and improving traceability.
- Protocol Optimization: Settings can be adjusted dynamically based on patient or scan needs, supporting consistency and quality.
- Analytics and Reporting: The devices facilitate robust quality assurance, performance analysis, and regulatory compliance.
- Remote Diagnostics: With remote technical support capabilities, connected injectors enable proactive maintenance to optimize uptime, seamless software integration and remote cybersecurity patching.
Jessica Starkey shared her real-world experience and highlighted operational motivators for adopting such systems, including reducing repeat scans, optimizing dose, and standardizing protocols. She noted that the ability to track and analyze events like contrast extravasations and waste has driven quality improvement projects and enhanced efficiency.
AI Solutions in Radiology: Enhancing Operational Efficiency and Workflow
Jason Johnson detailed the rapidly expanding scope of AI in radiology, emphasizing its impact on both workflow efficiency and clinical outcomes.
- Intelligent Worklist Distribution: AI can balance radiologist workloads in real time based on expertise and urgency.
- Automated Image Triage: AI flags urgent findings for immediate review, streamlining critical decision-making.
- AI-Powered Measurements and Reporting: Automation of segmentation, measurements, and structured reporting saves time and increases consistency.
- Follow-Up Detection: AI tracks follow-up recommendations, improving patient adherence and outcomes.
Selecting the right AI tools requires aligning them with clinical goals, validating performance, ensuring regulatory compliance, and prioritizing ease of integration and use.
Addressing IT Challenges and Cybersecurity
Implementing these technologies introduces new complexities for both connected injectors and AI. Panelists stressed the need for a robust IT infrastructure:
- Built-in resilience with manual fallback modes during connectivity loss.
- Local data storage on the injector with synchronization upon reconnection to minimize data loss.
- Cybersecurity measures such as end-to-end data encryption, multi-factor authentication, and regular security testing.
- Clear policies for data transfer, access control, and incident response.
- Business associate agreements and institutional approval processes to safeguard patient data.
The panelists unanimously agreed on the importance of engaging all relevant stakeholders from the outset to effectively address and overcome IT barriers. Drawing from her experience at UTSW, Starkey emphasized that fostering a strong partnership with the vendor played a crucial role in streamlining the implementation process.
Managing Workflow Disruption and Change
While introducing operational AI and connected injectors can temporarily disrupt employee workflows during implementation, the panelists provided actionable mitigation strategies:
- Hands-on training, peer champions, and reference tools to minimize learning curves.
- Early and inclusive stakeholder engagement to align goals and build buy-in.
- Transparent communication of benefits and addressing staff concerns proactively.
- Continuous feedback loops, role-tailored content, and ongoing training as technology evolves.
- Visible executive support to drive cultural acceptance.
Starkey emphasized that although the implementation required adding some mandatory fields and initial workflow adjustments, the disruption was minimal, especially with strong collaboration among technical supervisors, operations, quality managers, and clinicians.
Implementation Timeline and Long-term Benefits
Implementation durations vary by complexity, but base minimum timeframes include:
- Connected Injectors: 1-3 months
- Basic AI Tools (e.g., scheduling or triage): 2-3 months
- Workflow-Integrated Solutions: 3-12 months
- Comprehensive AI Ecosystems: 18-24 months with phased rollout
Initial impacts include training requirements and potential inefficiencies as staff adapt. However, the benefits — such as improved patient throughput, optimized contrast delivery, and reduced staff burnout — quickly outweigh the short-term adjustments.
Measuring Success: Key Metrics and Data Utilization
Connected injectors provide a wealth of operational data, including metrics tied to:
- Injection accuracy and consistency.
- Pressure monitoring for safety.
- Success and repeat injection rates.
- Operational uptime and error frequency.
- Contrast utilization and protocol adherence.
Starkey shared real-world applications, such as projects to reduce extravasations and contrast waste, and the presentation of injector data in operational meetings. These initiatives have led to decreased repeat scans, improved patient safety, and potential revenue enhancements.
Return on Investment: Building a Case Without Reimbursement
Although these innovations aren’t currently eligible for reimbursement, panelists provided a framework for prospective outcomes justifying investment:
- Opportunity for cost savings through potential to reduce errors, automate routine manual tasks, and optimize workflow.
- Ability to support patient experience with impacts to wait times and time-to-diagnosis.
- Potential to enable diagnostic capabilities, contributing to early intervention for high-risk patients.
- Plus, additional intangible benefits such as encouraging staff morale and readiness for future innovation.
Preparing for Regulatory Change: CMS’s ExRad eCQM Reporting
Looking ahead, radiology departments should start preparing now for new CMS quality reporting requirements. Bayer’s collaboration with Alara Imaging supports compliance by converting imaging data into CMS-compatible formats and integrating these processes with existing EHR, RIS, and PACS systems. Early adoption is encouraged to meet mandatory ExRad eCQM reporting by 2027, which will ensure alignment with national radiation safety standards.
Takeaways
The panel showcased that the future of radiology will need to embrace smart technology and data-driven practices. While implementation demands planning, collaboration, and investment, the potential outcomes include streamlined efficiency, focused patient care, and a foundation for ongoing innovation. As healthcare continues to evolve, radiology departments equipped with connected injectors and applications that drive operational efficiency can discover and harness opportunities for improving patient experience and operational excellence.
For more information on Bayer in Radiology’s connected smart injector solutions, visit:
https://www.radiologysolutions.bayer.com/medrad-centargo-ct